3D Systems说,3D打印技术将颠覆医疗行业规则
3D打印技术在医疗领域的应用可以追溯到光固化成型技术刚刚诞生的那些日子,甚至是更早。最近,我同一位工程师闲聊,他向我详述了20世纪80年代早期的那段经历。当时,诞生于20世纪70年代晚期的计算机断层扫描技术刚刚出现,他们通过“增材工艺”创造了较为粗糙的解剖模型。
CT扫描类似于为物体拍摄X光片。早期的X光片上的层切影像是用一张塑料薄片手工裁切而成的,而一个解剖物体的粗略3D模型就由这些连续的影像堆砌而成。这就是在3D打印技术发明之前人们制作3D解剖模型的方法。
Chuck Hull是光固化成型技术的发明人,也是3D Systems公司的创始人和首席技术官。他可能不曾想到他发明的这项技术会成为颠覆医疗领域的强有力的工具。该技术对医疗行业产生了重大影响,并将在未来使医疗领域受益匪浅。然而,要达成这些目标,需要使用更为先进的技术——我称之为“支撑技术”。不过,我们首先要检视历史,这样才能识别出那些能让我们迈向未来的支撑技术。通过“以史为鉴”,我们就能辨识出那些真正有助于实现3D打印医疗应用的支撑性技术,从而发现整个拼图中缺失的部分。
帮助我们实现现有医疗应用的关键“支撑技术”包括:
· 立体医疗影像技术的诞生(CT诞生于20世纪70年代、核磁共振成像MRI诞生于20世纪80年代);
· 3D打印技术的诞生(也被称为“增材制造”);
· 生物相容性材料的诞生(1996年左右,英国阿斯利康公司研发出Stereocol材料,Huntsman公司和3D Systems公司紧随其后);
· 触觉设计工具的诞生;
· 锥形束计算机断层扫描技术的诞生(2000年左右,主要应用于头部及颈部);
· 结合个性化仪器的虚拟外科手术方案的广泛应用;
· 3D打印技术在生物相容性金属上的应用;
· 活细胞生物打印技术用于人类器官移植。
毫无疑问,立体影像技术和3D打印技术在实现现有3D打印医疗应用方面发挥着基石的作用。这两大革命性技术的结合能够创 建出与实体大小相同的3D模型,并在实施重大再造手术前模拟整个手术过程。这些模型可以帮助外科医生更好地进行术前准备,并在手术过程中做出更优决策。更为重要的是,它可以在减少手术时间的同时改善病人的术后恢复情况。这些解剖模型还可作为个性化植入物的设计基础,可应用于从头骨到脚踝的全身的各个部分。在这一领域,全球越来越多的外科医生开始使用3D Systems公司出品的Medical Modeling医疗模型,其使用频率远超其他“触觉”技术外科手术指导工具。
生物相容性材料诞生于20世纪90年代中期,当时就已经展现出应用于真实手术的可能性。它将3D打印技术从单纯的诊断及方案设计工具转变为手术指导工具。
触觉设计工具在21世纪早期成功实现商业化,这使得大量繁杂的器官形状设计工作变得简单直观。一夜之间,设计师们发现了触觉医疗设计领域的创新应用,他们创造出之前无法想象的可自由变换的设计。
锥形束计算机断层扫描技术
就头部及颈部外科手术而言,锥形束计算机断层扫描技术对于3D打印技术应用的影响无疑是最大的。这是一台较小型的医院用CT扫描仪,它是医生办公室的一项标准配置。此类设备的扫描速度很快,价格也十分合理,辐射量也低于普通的CT扫描仪。它改变了口腔正畸、口腔外科和颌面外科等领域的诊断成像技术,正在全面影响口腔综合科。立体医疗影像数据的迅猛发展使得3D打印金属植入物技术、隐形正畸设备,以及正颌手术中使用的3D打印咬合片等医疗工具得到了更为广泛的运用。
可植入金属的增材制造技术诞生于21世纪头一个十年的中期,电子光束及激光技术促成了这一技术的实现。目前,钛金属、钛合金和钴铬合金植入物等以多孔几何体为主的产品占整个3D打印金属市场的比例还很小,但其增长速度极为迅猛。与此同时,3D打印的产量正在稳步上升,质量也在逐步提高,而部件的成本还在不断下降。这一趋势表明,金属打印将在未来十年对关节替换和创伤医疗设备的成品制造业产生重大影响。

虚拟手术方案及手术模拟设备使手术更加安全有效
虚拟手术方案结合了在计算机中针对手术过程的精确计算方案,以及可将虚拟方案真实运用到手术室的定制设备。虚拟手术方案充分考虑了在实施截骨迁移或替换其他骨骼或植入物的过程中外科医生可能遇到的情况。利用虚拟手术方案,外科医生在使用设备进行截骨时,能使截骨部位与病人的骨结构相适应,并帮助外科医生精准下刀,确保截骨过程与数字化方案完全一致。
“生物打印”目前还只是一个专业术语,指的是将活细胞作为打印材料的支架打印或真实3D生物结构打印。这些新兴功能为我们开启了无限的可能,使我们能够将细胞存入无限复杂和“活着”的3D结构。美国康奈尔大学的研究人员正在使用活细胞通过3D打印生成耳朵,而美国维克森林大学的研究人员正在研究利用病人的细胞来生成替代器官,减少对捐献器官的依赖,降低移植器官的排异几率。
3D打印医疗设备的市场前景远比大多数人意识到的更好,并且发展迅速。每年,牙科、口腔正畸和助听器行业利用3D打印技术制造出数以百万计的针对不同病人的个性化产品。在口腔正畸领域,这些技术对手术产生了多方面的影响,最为显著的影响包括两个方面:首先是定制植入物和手术设备的使用,其次是成品植入物的生产。光是口腔正畸手术的3D打印应用,每年所覆盖的病人数量就超过了15万人。
外科应用重建技术中心(CARTIS)
外科应用重建技术中心(CARTIS)位于威尔士的加迪夫,该中心在定制契合每位病人数据的个性化3D打印手术指导及植入物方面有着卓越的贡献。通过设计人员和外科医生的通力合作,他们证明了我们可以降低因复杂的外科手术而造成的创伤,并且使手术更快、更成功。
病人的同一可用3D数据使得虚拟手术方案取得了重大提升。
纽约大学Langone医学中心已经使用3D技术进行了多次手术,其中最著名的是被称为“一天还您完好下巴”的项目。该项目在非常关键的下巴手术方案中使用了3D Systems公司的虚拟外科手术方案(VSP)以及SLA光固化成型技术。该项目能够让患有下颌骨或上颌骨肿瘤的病人在入院的一天后即可完好无缺的办理出院手续。出院后的病人将拥有一套功能完整的健康的下巴和牙齿。整个过程采用了先进的虚拟外科手术方案,创建了个性化的手术工具和定制牙齿。该项目的理念是:只用一次手术就能重建病人缺失的功能,而以往这一过程通常需要经过好几次手术才能完成。
3D数据的使用还加速了面向外科医生的触觉模拟技术的突破性进展,这一情况与面向飞行员的飞行模拟技术很像。Simbionix公司的Procedure Rehearsal Studio(PRS)工作室利用个人医疗影像数据成功创建了仿真的医疗过程模拟场景。
通过将此项技术与现有的虚拟外科手术方案相结合,就能设计出一套全数字化的外科手术准备和执行流程。在不远的将来,外科医生可以将CT扫描数据导入外科手术方案软件,然后非常真实地模拟出整个手术过程,并迅速生成3D打印设备或模板,实现数字化方案到手术室的无缝切换。这一切还远吗?至少我还不这么认为。
未来愿景
那么,未来到底会如何?到底是什么样的“支撑技术”会促使3D打印医疗技术的进一步创新?它们又将产生怎样的影响?我相信有很多技术进步都将在其中扮演重要的角色。
首先,我期待看到3D打印技术从现在的硬组织(骨骼)再造手术应用发展到更多的器官、乃至其他的软组织应用上。事实上,3D打印技术的软组织应用已经成为了一个热门话题。美国新奥尔良杜兰大学的教授们正在研究如何创建可用于手术实践的真实人类器官模型,比如研发出与真实的肾脏具有同等柔软触感的材料,这样外科医生就能在手术前进行实战演练。现在的很多手术已经开始使用机器人外科手术辅助系统。机器人技术的出现将使外科手术更加自动化且更加精确。这将使我们能够迅速地从传统手术流程转向数字化手术流程,提高对精确手术方案的需求。

受益于突破性的CHAM数字化外科手术技术的菲律宾连体婴儿
其次,当这些技术变得更加成熟且成本降低的时候,我们将会看到3D打印医疗技术实现大规模的本地化。在未来十年内,我们有望看到这些便利的3D打印功能在大型医疗机构或当地医疗诊所中被日益频繁地使用。如今,外科医生和医学院已经开始重新设想外科医生的工作台。人们开始意识到,医疗从业人员的工作已经越来越离不开3D打印工具、用于直观设计的触觉建模工具和虚拟手术方案工具。
最后,我相信仿生设计将是下一个前沿技术。在未来的十至十五年间,我们会发现目前的臀部、膝盖、脚踝和肩膀的替代物实在过于粗糙落后。我们正在开发创新的更具说服力的设计方法。这是一种由身体及其需求所推动的设计语言。这将导致新型植入物的诞生。这一全新的植入物将根据设想的相邻组织之间的压力和拉力进行设计,能够对其功能和机械属性进行全面优化。
目前的3D打印医疗应用是激动人心的,但是当我们将其与未来技术相比较时,就显得较为平庸了。当我们将这些在不远的将来即将实现的不可思议的技术相互结合起来,并且将其应用于医疗领域时,我们将释放出3D打印全新的足以改变我们生活的强大功能。在3D打印技术各种不可思议的应用中,医疗应用是跟“人类”最为息息相关的。在接下来的十年内,我们将见证这一“人类”技术深入到我们周围数以百万计的人们的生活之中。
文章来源:TCT Magazine (转载请注明出处)
关于TCT
TCT建立于上世纪90年代快速成型(Rapid Prototyping)技术诞生之时,最初其名字为“快速新闻”(Rapid News), 后改为Time Compression Technologies,简称TCT。TCT品牌系列涉及纸印杂志、网站、展览和会议。20多年来, TCT杂志始终是3D打印、增材制造和产品开发技术跨终端用户、企业和工业应用的资讯“宝典”;TCT Show + Personalize母展每年在英国伯明翰举行,作为全球行业领先的增材制造、3D打印产品与技术展览会,自1995年至今已经成功举办了19届,每年的TCT都会吸引超过200个展商,10,000名专业观众前往。2015年3月,TCT将强势登陆中国上海,展会命名为TCT + Personalize Asia,中文名为亚洲3D打印、增材制造展览会暨TCT亚洲峰会(简称TCT 亚洲展),5,000平米的展区,预计将吸引到 100+ 参展商,5,000+ 专业参观者参与,将成就国内领先的3D打印和增材制造专业展览会;TCT已经成为全球行业用户、专家、厂商、顾问、思想领袖聚集的大社区和平台,不断推动增材制造和3D打印产业的发展。
原文:
3D printing medical breakthroughs are driven by enabling technologies and developments in other, typically unrelated, disciplines.
Medical applications of 3D printing technology date back to the earliest days of stereolithography and, if you can believe it, even earlier. Just recently, I sat with an engineer who recounted times during the early 1980s, after the advent of computed tomography (CT) in the late 1970s, when they would create crude anatomical models through an “additive” process.
CT scans are akin to x-ray slices of an object. In the ‘old days’, one would take a sheet of plastic and cut out, by hand, the cross sectional image from a piece of x-ray film. Stacking successive sheets one on top of each other would form a crude 3D model of an anatomic object, and this is exactly how it was done before 3D printing was invented.
Chuck Hull, the inventor of stereolithography and founder and Chief Technology Officer of 3D Systems, probably didn’t imagine Stereolithography as a game-changing tool for the medical industry, but it has had a tremendous impact on healthcare and promises even greater benefits in the future. Achieving these greater gains, however, will require utilising further technologies—I call them “enabling technologies.” Yet, to identify the enabling technologies that will propel us into the future, we must look to the past. With the benefit of hindsight, we can identify the supporting technological advances that first enabled medical applications of 3D printing, and start to recognise the puzzle pieces still missing.
The key enabling technologies that have brought us to our current medical applications include:
·The advent of volumetric medical imaging (CT in the 1970s, MRI in the 1980s),
·The advent of 3D printing (also known as “additive manufacturing”),
·The advent of biocompatible materials (circa 1996, Stereocol by Astra Zeneca in the UK, later Huntsman and 3D Systems) as well as laser sintering in nylon,
·The advent of haptic-enabled design tools,
·The advent of cone-beam computed tomography (for head and neck use, circa 2000),
·The widespread use of virtual surgical planning combined with personalised instrumentation
·The advent of 3D printing in biocompatible metals, and
·The bioprinting of living cells for replacing human parts with human parts.
Volumetric imaging and 3D printing are obviously the foundational technologies in enabling current medical applications of 3D printing. Combining these two revolutionary technologies together places life-size, physical 3D replica models into surgeons’ hands before major reconstructive surgeries. These models help surgeons better prepare for surgery, make better decisions during surgery and, most importantly, help improve patient outcomes while reducing surgical time. These anatomical models also became the basis for the design of personalised implants for areas ranging from the skull to the ankle. 3D Systems Medical Modeling is used by more surgeons worldwide in this area than any other for “tactile” surgical guidance.
Biocompatible materials emerged in the mid-1990s and opened up the feasibility of taking these tools into the operating theatre, transforming outputs of 3D printing from mere diagnostic and planning tools to surgical guides.
Haptic-enabled design tools were commercialised in the early 2000s, making the hugely labourious process of designing organic shapes simple and intuitive. Overnight, designers discovered new applications in haptic-enabled medical design, creating freeform designs that were impossible to imagine before.
Cone-Beam Computed Tomography (CBCT)
In the head and neck surgical specialties, no bigger invention has impacted the use of 3D printing than Cone-Beam Computed Tomography (CBCT). This is a smaller version of a hospital CT scanner, designed and priced to fit within a doctor’s office. Quick, affordable and with much less radiation than a typical CT scan, these devices have transformed diagnostic imaging for specialties like orthodontics, oral and maxillofacial surgery and are now impacting general dentistry. The explosion of volumetric medical image data has enabled broader access to medical tools like 3D printed dental implant drill guides, invisible orthodontic devices and 3D printed occlusal wafers used in orthognathic surgery.
Additive manufacturing of implantable metals emerged in the mid-2000s, made possible by both electron beam-based and laser-based technologies. Today, the production of titanium, titanium alloy and cobalt-chromium implants, focussed mostly around porous geometries, represents only a small percentage of the overall 3D printing medical market, but is rising quickly. At the same time, throughput of 3D printers is going up, quality of the parts is going up and cost of the components in production is going down. This trend means that metals printing is poised to make major impacts in manufacturing of off-the-shelf joint replacement and trauma devices over the next ten years.
Virtual surgical planning and surgical simulators help make surgery safer and more effective
Virtual surgical planning combines accurate, computer-based planning for surgical procedures in the computer with custom-designed, disposable instruments meant to carry the virtual plan from the computer to the operating room. Consider surgeons who cut bone for relocation or replacement with another piece of bone or an implant. Using virtual surgical planning, surgeons can use instruments for cutting a bone that fits along the patient’s bone structure and guides a saw-blade in a precise place, thus cutting the bone exactly as it was done digitally.
Bioprinting is typically used as a term today to describe either scaffold-based printing or true 3D biologic structure printing, using living cells as print materials. These emergent capabilities open up a new world of possibilities, allowing for the deposit of cells into infinitely complex and “living” 3D structures. Researchers at Cornell University, for example, are using live cells to 3D print ears. Researchers at Wake Forest University are looking at how to develop replacement organs using a patient’s cells, with the overall goal of reducing demand for donated organs and the rejection rates of transplanted organs.
The market for 3D-printed medical devices is larger than most people realise and growing rapidly. Dentistry, orthodontics and the hearing aid industries all rely on 3D printing to produce millions of patient-specific pieces every year. In orthopedics, these technologies are impacting surgery in many ways, most notably in the use of custom implants and custom instruments for personalised surgical procedures, as well as the production of off-the-shelf implants. All combined in just orthopedic surgery 3D printing touches more than 150,000 patients per year.
Centre for Applied Reconstructive Technologies
CARTIS, the Center for Applied Reconstructive Technologies in Surgery, in Cardiff, Wales, has been particularly successful in delivering 3D printed surgical guides and implants customised to a patient’s data. By having designers and surgeons work together, they have proved that complex surgeries can be less invasive, and with faster, more successful outcomes than before.
That same usable 3D data from the patient has allowed major advances in virtual surgery planning.
NYU’s Langone Center uses 3D technology on many procedures, notably one that they call ‘Jaw in a Day’ that allows the planning of critical jaw surgeries using a combination of 3D Systems’ VSP (Virtual Surgical Planning) and Stereolithography. ‘Jaw in a Day’ allows patients with large tumours of the mandible or maxilla to check into the hospital with a serious problem and check out the next day with a new tumour-free, functional jaw—complete with teeth. This process combines cutting-edge technology with virtual surgical planning to create disposable, personalised surgical tools and even custom-designed teeth—all meant to reconstruct the patient in a single procedure versus what’s typically taken several surgeries to accomplish in the past.
Use of 3D data has also fuelled breakthroughs in touch-based simulation for surgeons—not unlike flight simulations for pilots. Simbionix’s Procedure Rehearsal Studio (PRS), for example, utilises an individual’s medical image data to create an immersive, virtual simulation for a medical procedure.
Combining this technology with existing virtual surgical planning technology creates an entirely digital workflow for preparing and conducting a surgery. In a day not so far away, surgeons will be able to take a CT scan, import it into a surgical planning software, simulate the procedure in a very realistic way and then quickly output 3D printed instruments or templates to enable a seamless transfer of the digital plan to the surgical theater. Far-fetched? I don’t think so.
Future vision
So what is ahead? What are the enabling technologies of tomorrow that will drive further innovation in 3D-printed medicine and how will they impact the space? I believe a number of developments will play a key role.
First, I expect to see 3D printing move from today’s uses for hard-tissue (bone) reconstructive procedures to more work in organs and other soft tissues. In fact, work in soft-tissue 3D printing is already becoming a topic of conversation. At Tulane University in New Orleans, professors are working out how to recreate realistic human organs for practice models. This means developing materials that resemble the softer feel of, say, a kidney, so that surgeons can practice their surgeries before performing them. Many of these procedures are starting to use robotic surgical assistance. The rise of robotics will bring greater automation and control to surgical procedures—an important factor considering our rapid shift from traditional to digital surgical workflows and further compelling the need for accurate surgical planning.
Formerly conjoined Filipino twins benefitted from digital surgical advances at CHAM
Second, as these technologies become more sophisticated, and price points continue to decline, we’re going to witness a large-scale localisation of medical 3D printing. Within one decade, expect to see push-button 3D printing capabilities used with increasing frequency at hospital facilities and even your local surgeons’ office. Already, surgeons and medical schools are beginning to reimagine the surgeon’s desktop, understanding that no practitioner’s workspace will be complete without 3D printing, haptic modeling for intuitive design and virtual surgical planning tools.
Finally, I believe design to mimic nature is the next frontier. In ten to fifteen years from now, we will view today’s chunky, non-anatomic-looking hip, knee, ankle and shoulder replacements as primitive. We are in the process of developing a new, more eloquent design methodology—a design language powered by the body and its needs. This will give rise to a new genre of implants, designed with the stress and strain of adjacent tissues in mind and optimised for both functional and mechanical properties.
Until now the healthcare applications for 3D printing have been exciting, but they pale in comparison to what’s to come. When we combine the incredible technologies available to us in the near tomorrow and apply them to the medical field, we will unleash new, powerful and life-altering capabilities. Of all the incredible applications of 3D printing, healthcare is the most “human” of all. And in the next decade, we will see this “human” technology touch the lives of millions of our fellow humans.
http://www.tctmagazine.com/3d-systems-3D-printing-changing-the-game-in-healthcare-and-medical/
(责任编辑:admin)

 3D打印黄金吊坠让人们铭记
3D打印黄金吊坠让人们铭记 令人惊艳的3D打印喷气飞行
令人惊艳的3D打印喷气飞行 全球PK 3D打印PPSU,SOLVA
全球PK 3D打印PPSU,SOLVA 看3D打印自动化单元如何在
看3D打印自动化单元如何在 大型高精度电子结构件产品
大型高精度电子结构件产品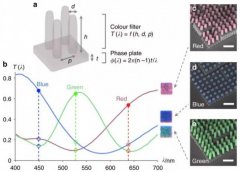 新型防伪技术:同一束光照
新型防伪技术:同一束光照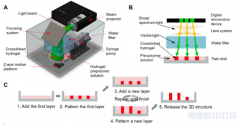 用于细胞3D打印的
用于细胞3D打印的

